Discover postsExplore captivating content and diverse perspectives on our Discover page. Uncover fresh ideas and engage in meaningful conversations
Precision Meets Innovation: Custom Mold Makers in McDowell County
When it comes to manufacturing high-quality plastic components, expertly designed molds are the foundation of success. That’s why custom mold makers in McDowell County, such as Brown Tool & Mold, are leading the way with cutting-edge design and engineering processes tailored to meet diverse industry needs. For more information please visit : https://www.slideshare.net/sli....deshow/precision-mee
GO2™: A Smarter Solution for Water Treatment Chlorine Dioxide Applications
When it comes to effective and reliable disinfection in wastewater treatment, water treatment chlorine dioxide has proven to be a superior alternative to traditional chlorine — especially in the form of GO2™. GO2™ acts as both a powerful disinfectant and strong oxidant, offering several key chemical advantages that enhance its performance in municipal and industrial applications. For more Information: https://www.slideshare.net/sli....deshow/go2-a-smarter
Suprano Displays stands at the forefront of the exhibition industry as a leading stand builder in Europe. With cutting-edge manufacturing facilities in Germany, the Netherlands, Italy, Poland, and Dubai, we deliver world-class exhibition solutions tailored to each brand's unique identity. For over a decade, our team has specialized in crafting fully customized, results-driven exhibition stands that captivate audiences and elevate brand presence. Whether you're preparing for a trade show, expo, or industry event, Suprano Displays transforms your vision into a high-impact, unforgettable experience. https://supranodisplays.com/
Hemoglobin Feed Market Future Growth Prospect, Industry Trends and Demand Analysis Till 2030 | #hemoglobin Feed
How To Bet On Table Tennis: A Step-by-Step Guide
Bet on table tennis with MGLion! Get your online table tennis betting ID and follow our step-by-step guide for smart betting strategies.
https://mglion.co/blog/how-to-bet-on-football/
The Definitive USA Passport Application Guide for First Timers
https://usa-passport-application.com
We will handle the entire USA Passport Application or renewal process for you, no guides needed. Submit your USA Passport Renewal Application, verify documents, and access the correct Passport Application Form USA seamlessly. Whether it’s your first submission or a renewal, our service ensures your Application for Passport USA is error-free and processed swiftly. Focus on packing; we will take care of the paperwork!
https://blog.usa-passport-appl....ication.com/the-defi
#passportrenewal, #uspassportapplication, #usapassportapplication, #applyuspassport, #applyusapassport,
#renewmypassport, #renewpassport, #applyforpassport, #replacelostpassport, #replacestolenpassport, #travelstatepassport,

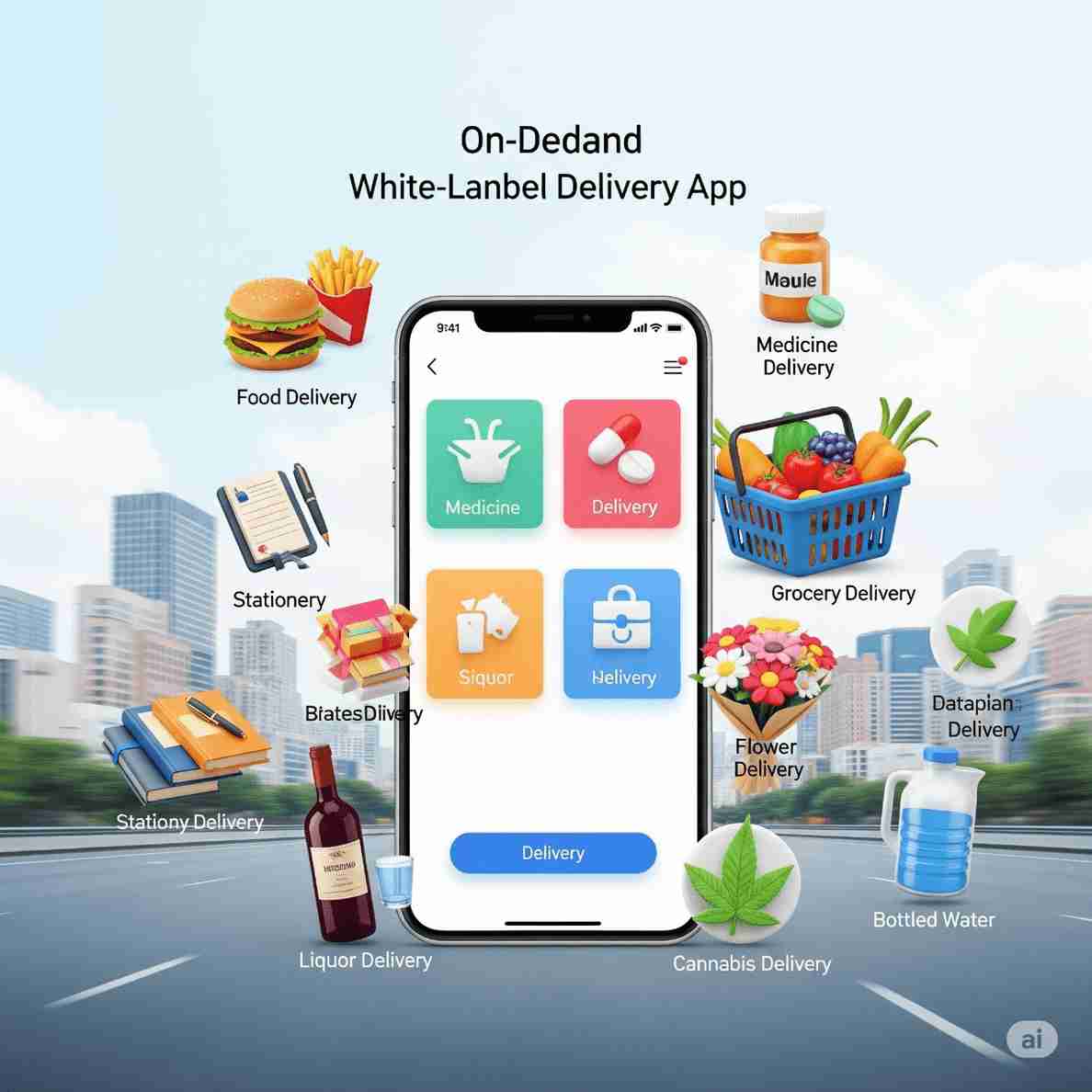
The rise of the digital economy has revolutionized how businesses operate, connect with customers, and deliver services. Among the most prominent advancements in this era is the concept of on-demand apps, which have become a game-changer for various industries. From ride-hailing to food delivery, home services, healthcare, and grocery delivery, on-demand apps have set a new standard for convenience and efficiency.
More Link: https://app-clone.com/white-label-delivery-app/
#whitelabeldeliveryapp #ondemandmultideliveryappclone #ondemandwhitelabeldeliveryapp #multideliveryapp #whitelabeldeliveryappclonescript #whitelabeldeliveryappsolution #ondemandmultideliveryappservices
Financial Management Software | Accounting software - CRM Online
CRM Online is one of the best online accounting software in the UK, that streamlines financial management across your entire organization.
https://www.crm-online.co.uk/i....ndustries/financial-